Excerpted and adapted from remarks delivered on May 20, 2022
I start with a question that is asked every day in our clinics and by all of you: Why?
A question for anyone who is diagnosed with a medical problem or a chronic condition. Why did this happen? Why now? Why me? At the University of Chicago Medicine Digestive Diseases Center, we ask many of the same questions too, but we also ask, “Why not?”
I ask every patient I see for their theory of how they developed inflammatory bowel disease. I am looking for the answer which will come if we listen carefully enough, follow that listening with hypotheses, and follow those hypotheses with clinical research, and follow that clinical research with laboratory research. Discovery of associations leads to discovery of new treatments, and discovery of causes leads to discovery of cures.
But how do you create a culture of inquiry, an expectation for new discoveries, and results that transform the effect of disease on a person and on their family, to disease control and an unrestricted quality of life?
The ingredients that have made the Digestive Diseases programs at the University of Chicago great are 1) the University itself, 2) our brilliant and dedicated faculty and staff, and 3) the amazing GI Research Foundation.
The University of Chicago was created as an institution of higher learning with, as University President Robert Maynard Hutchins said in 1931, “devotion to truth, the courage to be independent, an enthusiastic interest in the community and in new ideas, in intellect rigorously trained, and being trained.” Today is graduation day on campus, and during this special time each year, during the pomp and circumstance, the students and their families celebrate the completion of the journey that is ending, and the new one that is beginning.
At times like these, the rich history and legacy of the University of Chicago is celebrated, and we are reminded that we are part of a lineage of scholarship and critical inquiry in the service of a better society. This culture must be preserved by its faculty and safeguarded by those who come after them.
Our medical center grew out of the University and was developed with the same principles.
The medical center has been a part of the campus for almost one hundred years, and the core function of the University of Chicago Hospitals required commitment to the community and patient care, but always emphasized research to understand the mysteries of the human body. Among its first eight faculty hires was Dr. Walter Palmer, a physician scientist and son of a family practice doctor who had an interest in GI diseases. Dr. Palmer focused on research and discovery of the major GI problem of the day—peptic ulcer disease. In 1935, Palmer was joined by and then mentored a young physician, Dr. Joseph Kirsner. Shortly after starting his job with Palmer, Kirsner met a young woman with ulcerative colitis. A little-known condition at that time, she succumbed to her disease, and this had a profound impact on Kirsner. He subsequently devoted his career to understanding the causes and treatments for the inflammatory bowel diseases.
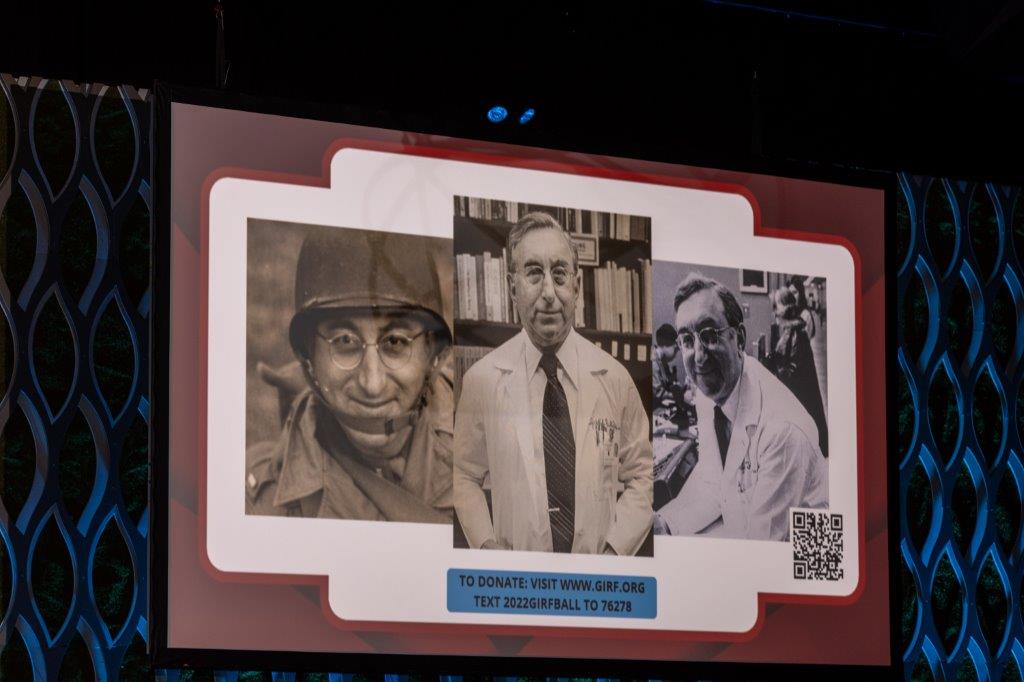
Joseph B. Kirsner, MD, PhD
By now the legacy of Kirsner is known to many of you—it is the reason the GI Research Foundation came to exist. The longer I work as a physician-scientist, the more I understand the impact this young woman had on him. As I think many in this room know, those of us who have dedicated our lives to medicine are deeply moved by the privilege of intimately knowing our patients and their pain, sharing the sadness of that which we cannot control, but also of celebrating the joys of success and finding inspiration to do it better for the next patient.
The second ingredient to our ongoing success is our UChicago people. Our amazing Digestive Diseases Center is now made up of over 300 physicians, scientists, trainees, nurses and staff. In the last year, we have been in more locations, seen more patients, performed more surgeries and published more scientific papers than ever before. Under the co-directorship of Dr. Mike Charlton and Dr. John Fung, our transplant center has performed more transplants in multiple organs than in the history of the institution. In the next two years, we expect to be in two more locations, one of which may be in a suburb near you.
When I meet with my faculty, I challenge them to tell me “What would make your program the best in the world?” (because if you don’t think about it, you will never get there). I tell them that they should work to solve the toughest problems, and I will work on getting them the resources. These conversations have led to our nationally recognized multi-disciplinary liver tumor clinic led by Dr. Anjana Pillai, our multi-disciplinary obesity initiative led by Dr. Mustafa Hussain, our cutting-edge interventional endoscopy program led by international leader Dr. Uzma Siddiqui, and most recently, our intestinal ultrasound program, which enables us to assess inflammation in the bowel, in real time, at the bedside.

Dr. Rubin receiving the Joseph B. Kirsner Award at the Champions for a Cure Ball
Our research teams have been incredibly productive as well, with more than 300 active human subject trials and hundreds of ongoing pre-clinical laboratory experiments. In the past year, Dr. Gene Chang and his colleagues have shown how the microbiome of infants may predict future immune diseases. This work is being explored in a massive grant in collaboration with the Chinese University of Hong Kong, and politics and pandemics allowing, he and I will be traveling there later this year to continue that work. Renowned immunologist Dr. Bana Jabri now leads the UChicago Human Immunology Institute, and this year, with Dr. Valerie Abadie, published groundbreaking work developing a mouse model of celiac disease, and Dr. Carol Semrad is leading our efforts to develop treatments that would allow people with celiac to tolerate gluten again. GIRF directly supported Dr. Noa Krugliak Cleveland’s work, which identified the potential for the bowel to remodel itself after healing from ulcerative colitis.
We are most fortunate to work with technically outstanding surgeons, who are also funded investigators. GIRF has supported two of our colorectal surgeons, under the leadership of Dr. Neil Hyman. Dr. Kinga Skowron-Olortegui received her master’s degree in public health sciences and Dr. Benjamin Shogan has received a competitive NIH career development award to study the role of bacteria in colorectal cancer.
But at the end of the day, it still comes back to the individual physician, the individual scientist, and their focus on the next individual patient. [Read remarks from Dr. Sonia Kupfer and Cambrian Liu].
The pressures of clinical medicine from a patient side are well known to you all—the advent of technological innovations, new treatments and surgical procedures have been accompanied by exorbitant costs of care, third-party payors coming between doctors and patients, and on the administrative side, increasing demands on the clinical teams to see more patients, do more procedures and generate more revenue. In addition, research funding has become more competitive to obtain, and the infrastructure to perform research has become more complex and expensive.
And so, the third critical ingredient to our success is you: the GI Research Foundation. Our friends at GIRF have stepped up time and again to address the needs of the physicians and scientists, and in the last eight years, have increased their support to meet the times. GIRF now provides GIRF Scholar awards to our faculty to protect their time to pursue otherwise unfunded academic priorities like early phase research, curriculum development, teaching our fellows, and quality of care efforts. GIRF supports our biobank, which we have renamed the GI Research Foundation Digestive Diseases Biobank. This includes the salary for our clinic and procedure unit technicians, our clinical research coordinators and support for the Director, Dr. Joel Pekow, and Associate Director, Dr. Valerie Abadie. Our digestive diseases biobank now has over 11,000 patients in it—and having this incredible resource makes answering many research questions simply a matter of going to the freezer.
In the past year, the Scientific Advisors to the GIRF Board, Dr. Michael Charlton, Dr. Gene Chang, and I, launched a new GIRF research grant funding process that included peer review by our scientists, physicians, and GIRF Board Members. The creation of this process has allowed us to move from ad hoc funding of individual projects to a formal grants process that allows our colleagues the opportunity to apply for and to secure the support necessary for pilot research projects. These are the projects which develop new hypotheses and higher risk initiatives to seed larger projects and make our teams more competitive for federal funding. In the first cycle of this exciting grant process, GIRF has funded seven of our colleagues, including Drs. Sonia Kupfer and Cambrian Liu.
In the last year, GIRF matched the contributions of two donors to launch our Community Health in Digestive Diseases initiative. Designed to provide digestive disease outreach to the communities in and around the University of Chicago in all its locations, the program is co-directed by Dr. Ed McDonald and Dr. Sonali Paul, and will explore the biological and social contributors to digestive illness in people of different racial and ethnic backgrounds. The connection between health and the social sciences, and the collaboration with our scientists in the microbiome institute is singularly unique and holds immense promise. We are immensely proud of this part of our mission.
Finally, GIRF has, as it always has, kept its eyes on the bigger picture as we have worked to develop our largest endeavor ever: our regenerative medicine program. As mentioned briefly last year during this Ball, regenerative medicine is the study of how tissues develop and mature into different organs, and how tissue injury occurs and changes with age or disease can be repaired or replaced. The potential applications for such a program are incredibly exciting, and may include tissue healing in inflammatory bowel disease, and organ regeneration in intestinal, liver, or pancreas failure conditions. Ultimately, these discoveries will yield new insights and treatments for GI cancer as well. An institution like the University of Chicago and its multitalented scientists and experts across different departments and specialties is the only place a program like this can be created and succeed, and with GIRF’s help, I know we will. Your support is critical to our missions. We appreciate your dedication and generosity. Thank you.