Everyone has overindulged or eaten a food that didn’t agree with them. For most people, this means that the next time they are offered spicy chili or rich dessert, they politely decline or make a different choice. But for patients with Crohn’s disease and ulcerative colitis, this experience can be all too common—if nearly every time you eat anything, it hurts, limiting what foods you eat makes sense. But it can also be a slippery slope, leading to extremely restricted approaches to food.
“We see patients who have severely restricted what they eat all the time,” explains Courtney Schuchmann, registered dietitian at the University of Chicago Digestive Diseases Center. “Sometimes they go online, and find what foods to avoid with diabetes or another unrelated condition…but often, they just restrict and restrict and restrict, and their group of ‘safe’ foods becomes smaller and smaller and smaller. Over time, this can result in an increased risk for weight loss, malnutrition, vitamin, and mineral deficiencies, because they’re no longer consuming adequate nutrients from their food intake. Their GI symptoms might be improving, but it could have consequences to their general health.”
 This type of eating restriction can also lead to eating disorders, a range of conditions in which there are persistent changes to eating behavior with negative impacts on physical or mental health. Or it can lead to disordered eating, which includes food- and diet-related behaviors which don’t necessarily meet the diagnostic criteria for eating disorders, but are still disruptive to an individual’s mental, physical, and emotional well-being.
This type of eating restriction can also lead to eating disorders, a range of conditions in which there are persistent changes to eating behavior with negative impacts on physical or mental health. Or it can lead to disordered eating, which includes food- and diet-related behaviors which don’t necessarily meet the diagnostic criteria for eating disorders, but are still disruptive to an individual’s mental, physical, and emotional well-being.
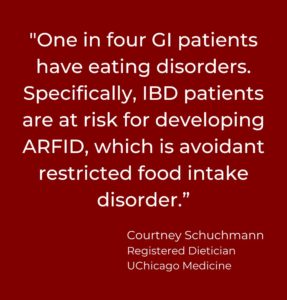
“IBD patients have a heightened risk of disordered eating, and one in four GI patients have eating disorders. Specifically, IBD patients are at risk for developing ARFID, which is avoidant restricted food intake disorder.” Explains Ms. Schuchmann. “We need to be aware of this as a community, and as providers.”
The social and psychological impact of these eating patterns can be significant. Some patients avoid situations that typically bring great joy and fulfillment, like eating with friends and family, going to restaurants, or gathering for birthday parties and holidays. Similarly, the guilt, anxiety, or worry associated with eating can be debilitating.
Ms. Schuchmann and other health care providers encourage patients to work with their health care team to ensure that their dietary behaviors are healthy, and supportive for them and their disease.
“We understand that when you have a digestive disease, restricting what you eat to some degree is a way of coping, and it’s a safety mechanism for a lot of people. But a healthy, sustainable diet is important for long term health. And we want to make sure you have all the support you need,” says Ms. Schuchmann.