By: Anna Gomberg, Administrative Director, IBD Center
Children and teenagers with Crohn’s disease and ulcerative colitis usually count on their parents to support them with the many aspects of living with a chronic disease: making appointments, keeping track of medications, and knowing when to call their doctor. But how do young patients learn to take on these responsibilities as they grow into adulthood?
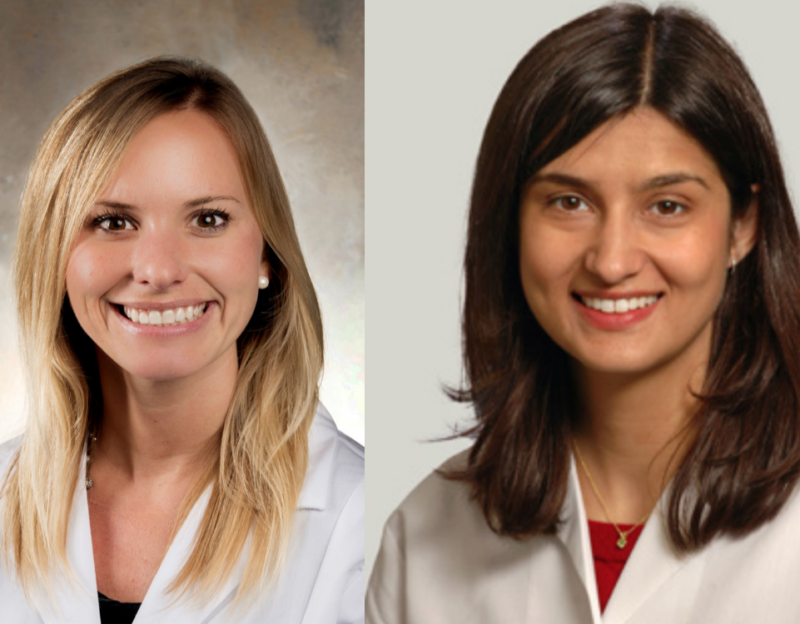
At the University of Chicago Medicine, there is a special program to assist young adult patients to be ready to take on all the tasks they will need to manage their disease independently. Run by Katie Sonnenburg, a pediatric nurse practitioner working in pediatric GI, and Sushila Dalal, MD, and adult gastroenterologist and Assistant Professor of Medicine, the Transition Clinic helps patients transition from pediatric to adult IBD care.
“As children and teenagers, patients often have their parents take care of their appointments, medications, communicating with their medical team. As they grow up, the patients themselves have to take ownership of their disease and do all of these things on their own,” explains Dalal.
“Patients can be diagnosed with inflammatory bowel disease at any age, but the most common time is during the teenage years. Sometimes, pediatric gastroenterologists and APNs see patients diagnosed at 5, 6, 7, 8 years old, and we get to know them really well. Then, when it’s time to start seeing an adult provider there’s a lot of anxiety from both the patient and the parent. Our idea is to help ease the transition and help the patient get to know their new provider and make sure there is a familiar face in the room.” explains Sonnenburg.
Pediatric and adult care for IBD differs in important ways. Crohn’s disease patients who develop the disease when they are younger sometimes have more severe disease, but also have not had the disease for as long as adult patients, and therefore may have sustained less damage from inflammation.
Pediatric patients do not undergo the same frequency of diagnostic procedures (adult Crohn’s disease and ulcerative colitis patients often undergo colonoscopies or other imaging annually), and procedures performed are sometimes done differently for pediatric patients. This means that a young adult patient may be undergoing a familiar procedure, but rather than receiving contrast given through a nasal gastric tube, they will be expected to drink a contrast for the first time. Or, they may experience sedation rather than general anesthesia. These are all important considerations for the transition team.
Often, parents require special guidance from the transition team as they learn to let go and trust their young adult child to manage his or her own care.
“It’s absolutely a transition for the parents as well,” says Dalal. “They have had a huge role in managing their child’s care and making sure they were scheduling their appointments and ordering their medicine, and it is really scary for a parent to let go of that. What if the patient doesn’t take their medication, and get sick? It can be very anxiety-provoking for parents. We understand that, and help them. We try to emphasize to parents that they are very actively involved in the process of transitioning with their son or daughter, because they have to teach all the things they have been doing. The parent’s role just changes to more of a mentor role. Maybe the child doesn’t even realize the many things a parent has been doing to help care for them.”
Sonnenberg and Dalal report that the ideal time to transition from pediatric to adult IBD care is before the patient goes away to college or starts out on their own.
Sonnenburg and Dalal work with families to put together a plan to stay on medications, keep up with prescriptions, make appointments for convenient times, work through insurance changes, follow up with their physicians, and find care locally. They then coordinate care with adult providers so that initial appointments are with the team as a whole.
Patients in adolescence face unique social and emotional challenges connected to living with a chronic illness, and the transition team can help to support patients as they deal with anger, sadness, or other negative feelings about having inflammatory bowel disease. In college or living on their own for the first time, these patients need are especially vulnerable to feeling alone They also may need support to continue with their treatment plans when their impulse might be to swim in uncharted waters: What happens if I don’t take my medication? Do I really have this disease, if I’ve been feeling well for a year or two?
“This is a normal part of development, and we understand that,” Says Sonnenburg.
One strategy employed be Dalal and Sonnenburg is shared Decision-making.
“There’s rarely just one option for patients getting treatment for IBD,” explains Dalal. “If a young patient says to me, I haven’t been taking this medication regularly, because it makes me feel tired or sick to my stomach, I can work with that and help to find a treatment plan that we can agree on. This can be very empowering for our patients. Says Dalal, “Really, we are here to help them grow and succeed during this exceptionally exciting time in their lives.”